Dr. Joseph Performs Endoscopic Decompression and Fusion with Coronal Correction
Dr. Sam Joseph continues to pioneer new techniques for minimally invasive spine surgery by implementing cutting edge techniques and utilizing the FlareHawk7 endoscopically assisted system.
CLINICAL PRESENTATION
The patient is a 52-year-old female with a longstanding history of severe lower back and right leg pain. She had failed therapy, medication and injections, and had a prior right-sided laminectomy at L4-5. The patient presented to another surgeon who offered her open lumbar laminectomy and fusion. She then presented to Dr. Joseph’s office for a second opinion for a less invasive approach.
EXAM
Severe lower back pain with palpation, spasm, pos SLR right side, decreased sensation L3, 4, 5, absent DTR right side.

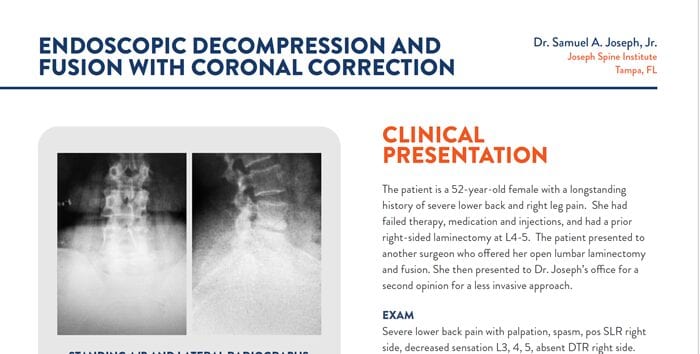
IMAGING
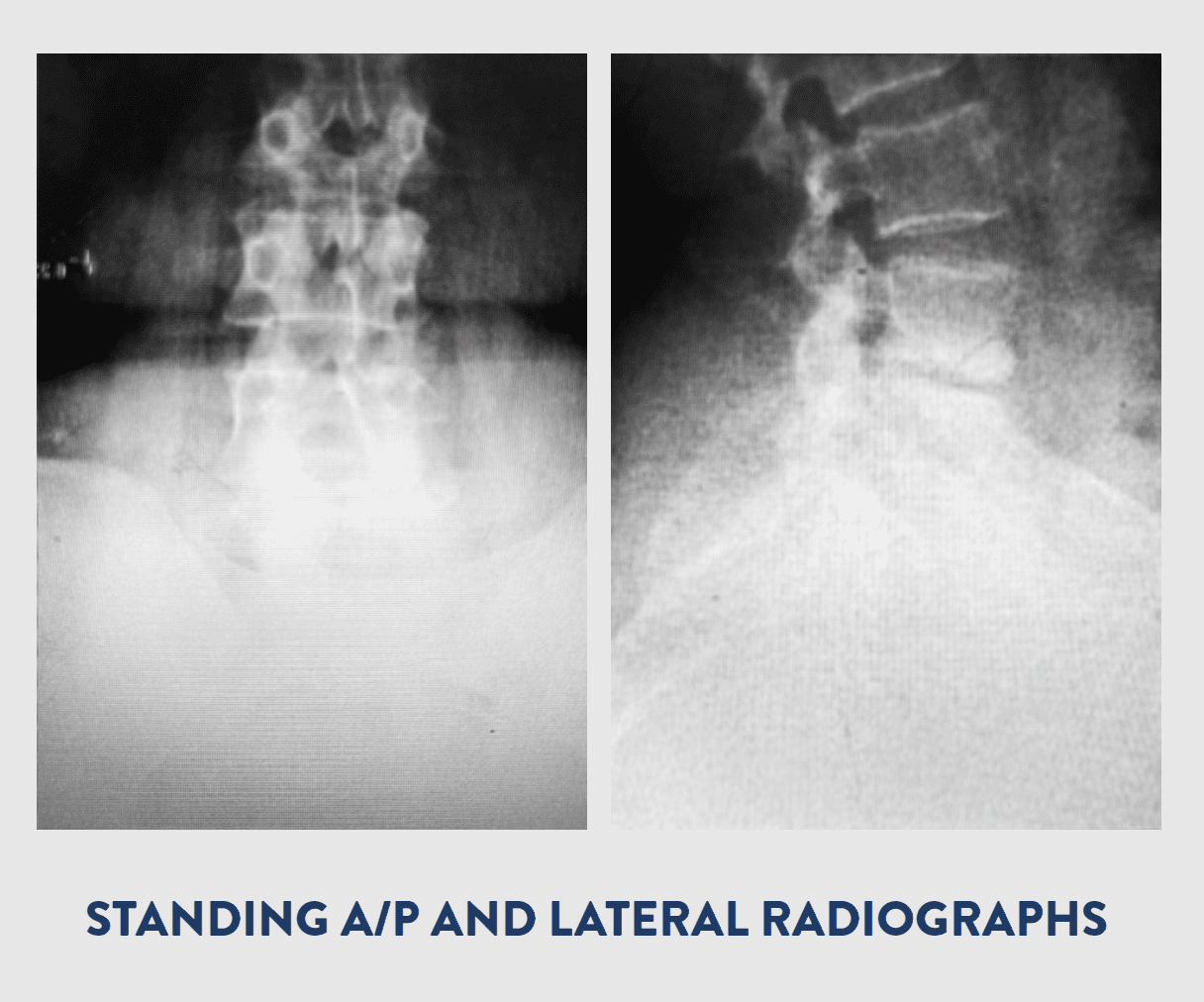
X-RAY
- Moderate spondylitic changes at L4-5
- Endplate degeneration identified
- Facet arthropathy identified
- Scoliosis curvature
- Exhale. Leave the pose incrementally. First, bend the arms slowly backwards. Lower the navel to the mat, then the chest, then the shoulders, and, lastly, the forehead.
MRI LUMBAR SPINE
- L2-3: 5 mm central disk protrusion is seen with bilateral facet arthropathy.
- L3-4: Dehydrated, bulging disc is seen with a 4 mm broad-based disc protrusion and bilateral facet arthropathy.
- L4-5: Dessicated, bulging disc and osteophyte and facet arthropathy are seen with a 7 mm right foraminal disc protrusion. Prior Laminectomy. Severe foraminal narrowing on the right side.
- Exhale. Leave the pose incrementally. First, bend the arms slowly backwards. Lower the navel to the mat, then the chest, then the shoulders, and, lastly, the forehead.
Modified Seated Spinal Twist
Modified Seated Spinal Twist
PROCEDURE
OVERVIEW
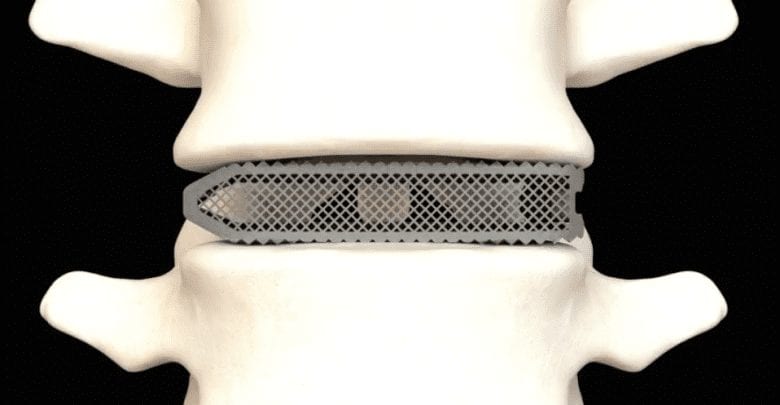
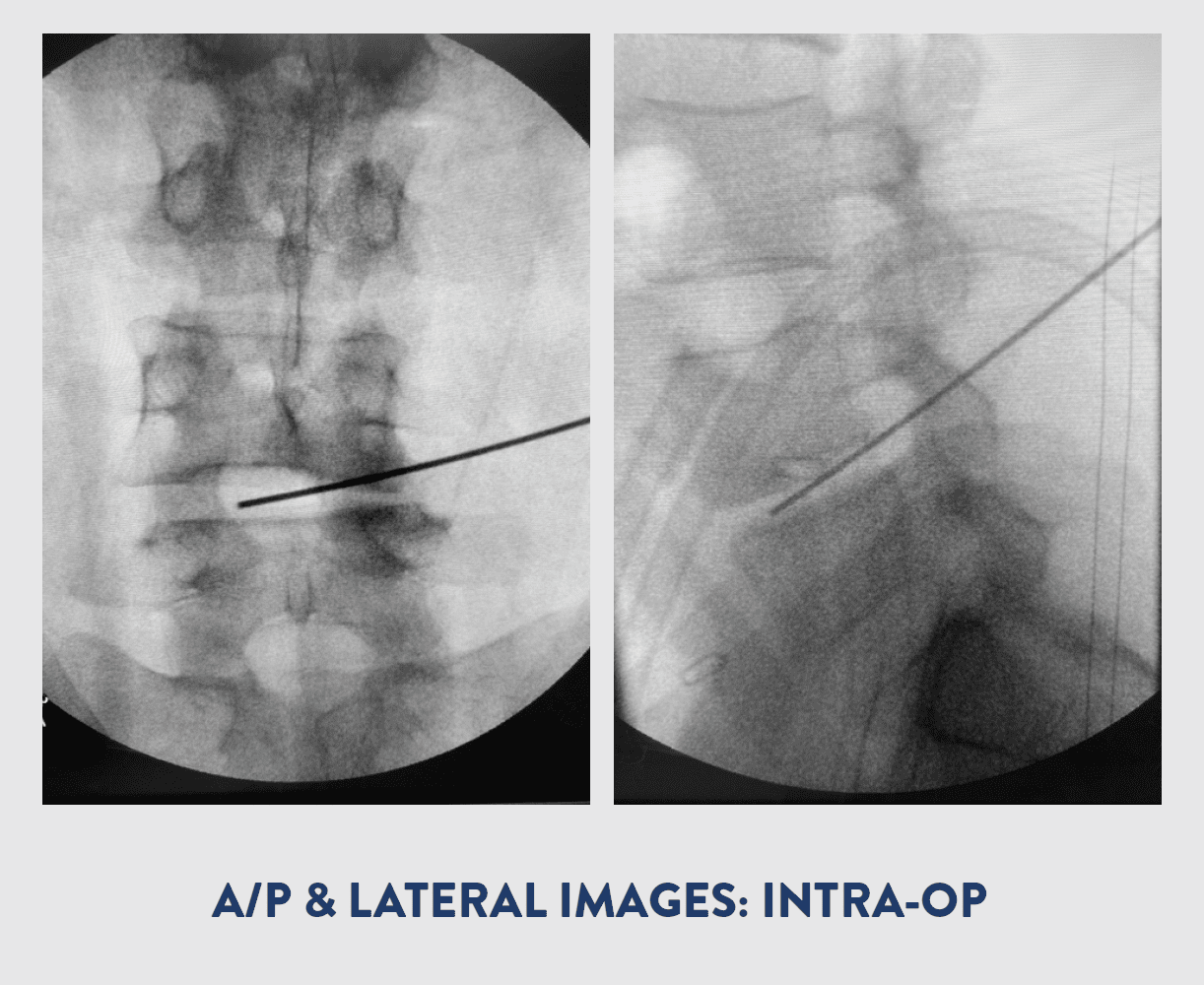
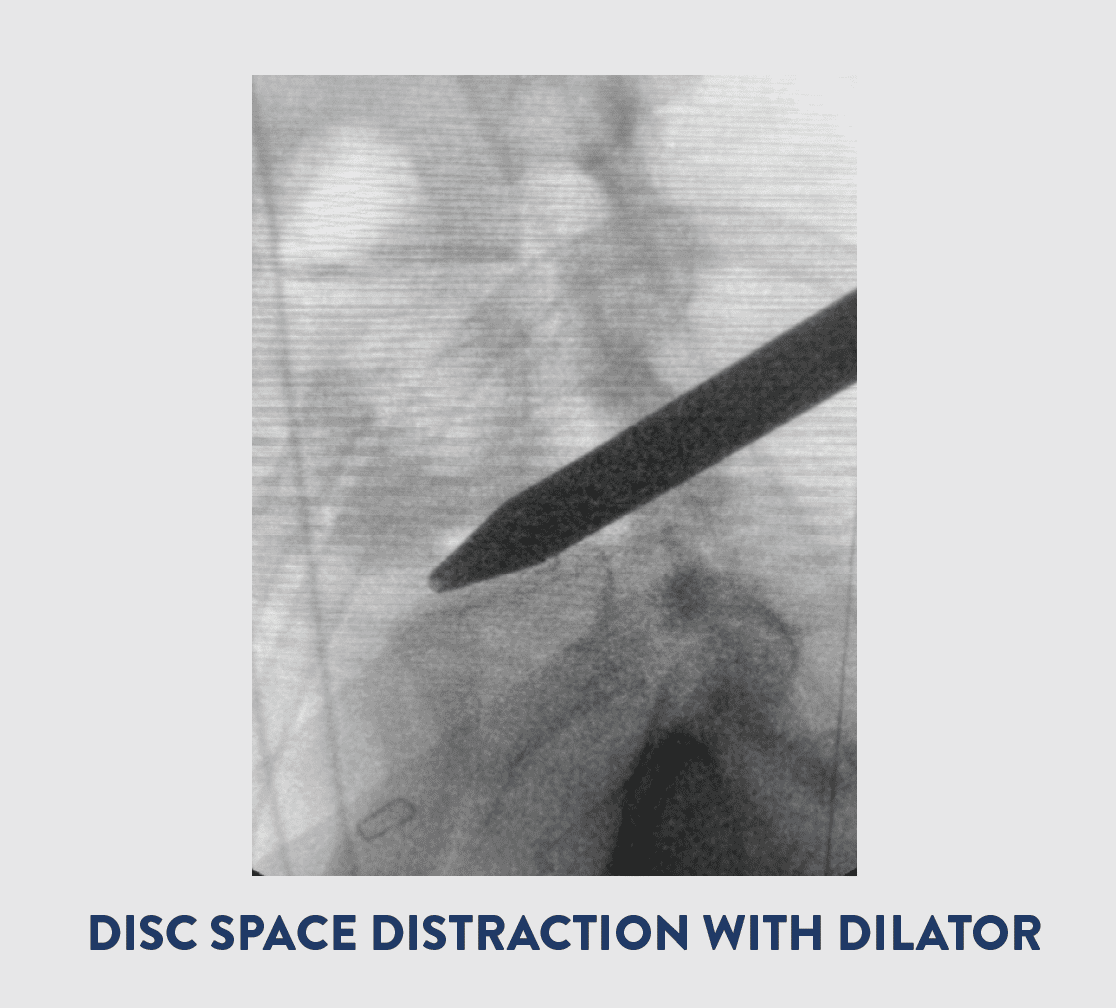
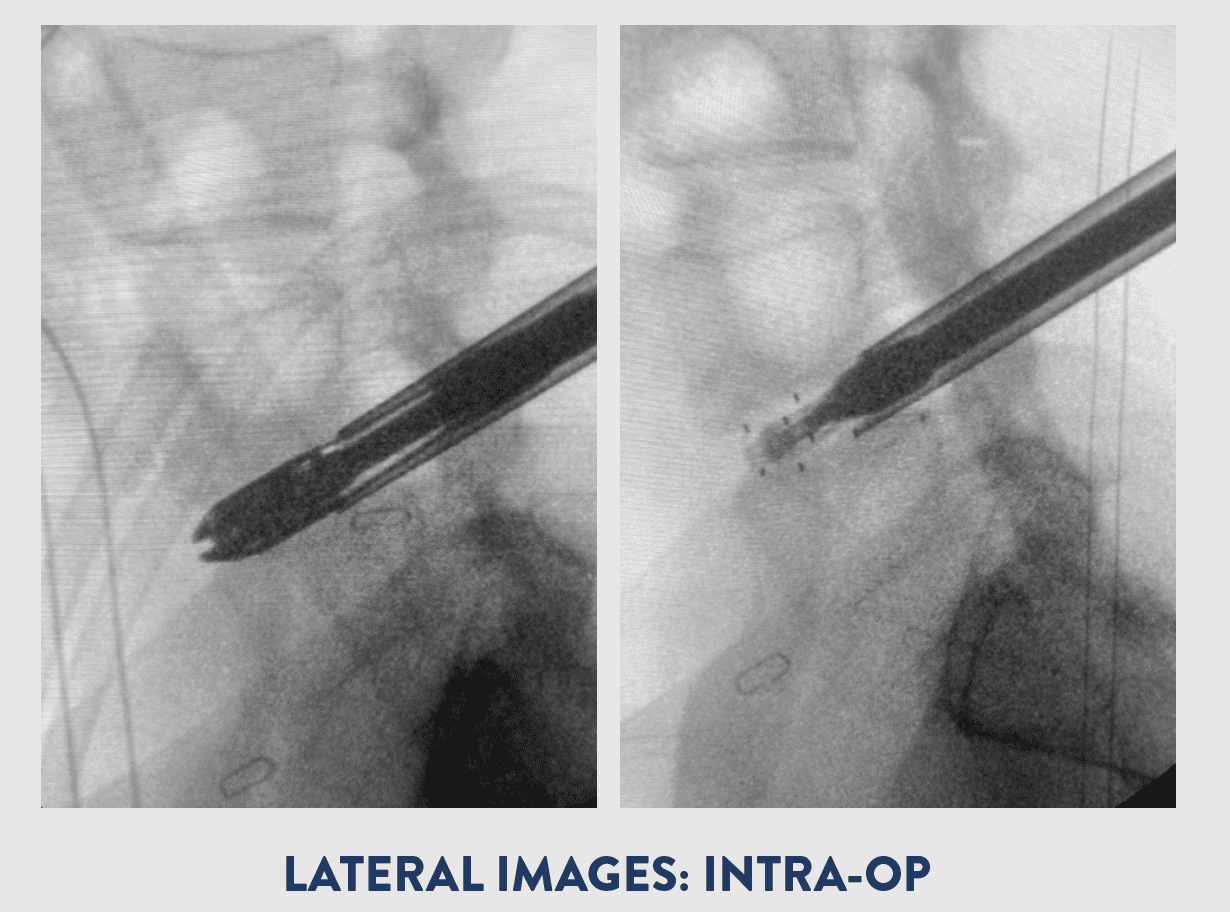
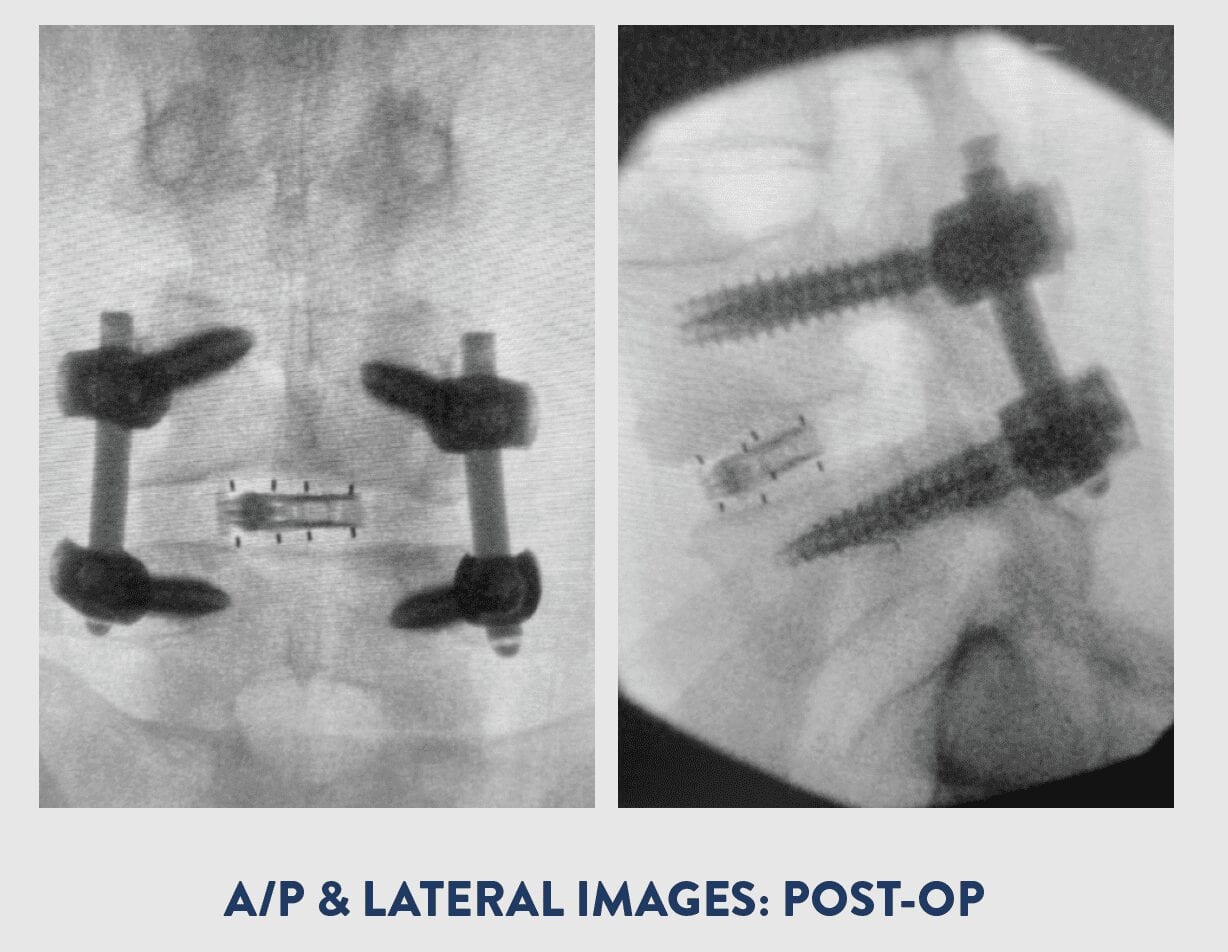
Dr. Joseph performed a right sided foraminotomy, discectomy, and partial facetectomy of L2-3, L3-4 and L4-5. An endoscopically assisted TLIF was performed on the right side of L4-5 with bilateral posterior pedicle screw instrumentation at L4-5.The FlareHawk7 endoscopically assisted system allowed Dr. Joseph to perform his discectomy and deploy an 11mm wide, 26mm long, 10mm tall Implant with 6° of lordosis through an 11mm Tubular Retractor.
BLOOD LOSS
50 cc
IMPLANT INSERTION PROFILE
7mm W x 7mm H x 26mm L
IMPLANT DEPLOYED PROFILE 11mm W x 10mm H x 26mm L with 6° Lordosis
PROCEDURAL RATIONALE
Endoscopic decompression with fusion was ideal for this patient due to her multilevel symptomatic foraminal stenosis as well as her scoliosis and prior Midline Laminectomy at L4-5. The Kambin’s triangle approach avoids the scar tissue from prior surgery. The round dilator acts like a distractor elevating the right side and the FlareHawk7 allows expansion to maintain the correction through a very small working channel. This allows both direct and indirect decompression at the L4-5 level.
OUTCOME
The patient had no more leg pain and only mild back soreness. Discharged home in fewer than 24 hours post-op. The patient continues to do well.