The Difference Between Minimally Invasive Spine Surgery vs. Traditional Open Surgery
written by Dr. Samuel A. Joseph, Jr.
Spine surgery has been transformed significantly by the growth of minimally invasive spine surgery (MISS) procedures. As a spine surgeon I am always researching new ways to improve patient outcomes. Implementing new advancements that improve recovery time, create less scaring and less pain after an operation is the ultimate goal for all of us at Joseph Spine Institute. By combining advanced techniques and partnering with with innovators developing cutting edge spine technologies patients now have more options for minimally invasive spine surgery and outpatient procedures than ever before.
Is Minimally Invasive Spine Surgery Right for You?
Many patients come in to my office confused about the difference between open surgery and minimally invasive spine surgery otherwise called MIS. The traditional open surgery is still necessary in certain situations. However, with the advancement of newer technology most procedures can now be performed in a MIS manner. There are many factors involved in this decision, most importantly are the specific details of your condition. Consulting an exceptionally trained and well respected board certified spine surgeon is of the utmost importance when determining the type of treatment options that are best for you.
What Is Open Spine Surgery?
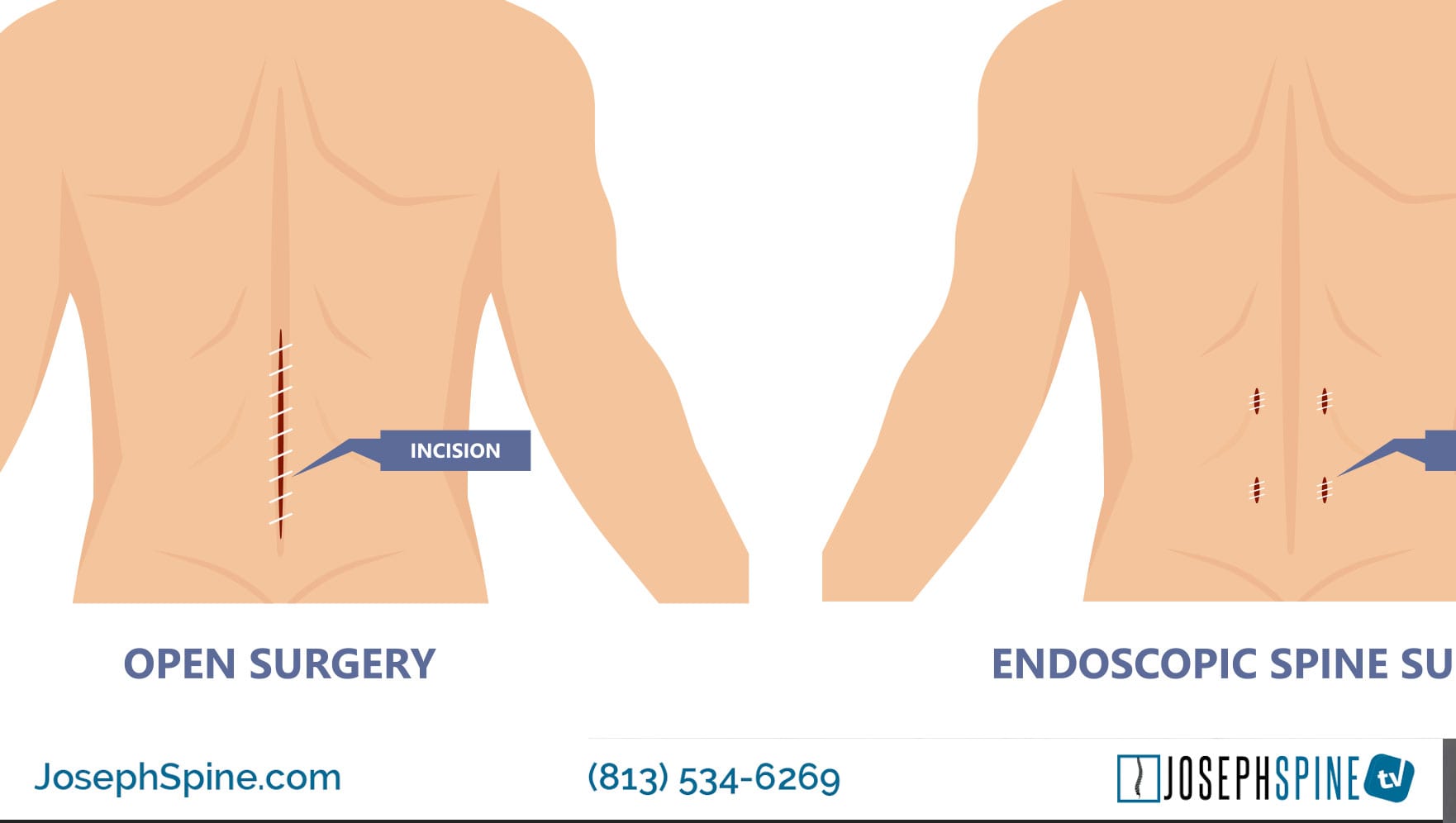
During open surgery, you can expect to be opened up (hence, the name). Open surgery involves making an incision that then proceeds down to pull the muscles and ligaments off the spine to get access to the problem area. This is typically done in a hospital and requires an overnight stay. It’s also possible that, during an open procedure, muscles and tendons will have to be cut through and moved aside to reach the affected area. This can cause damage to these tissues, possible large loss of blood and prolong recovery.
Once bones of the spine can be visualized, the necessary spinal procedure can begin. Most open spine surgeries require the following:
- Anesthesia
- Large incisions
- Muscle retraction
- Long surgery times
- Hospitalization
- Long recovery times
What is Difference with Minimally Invasive Spine Surgery?
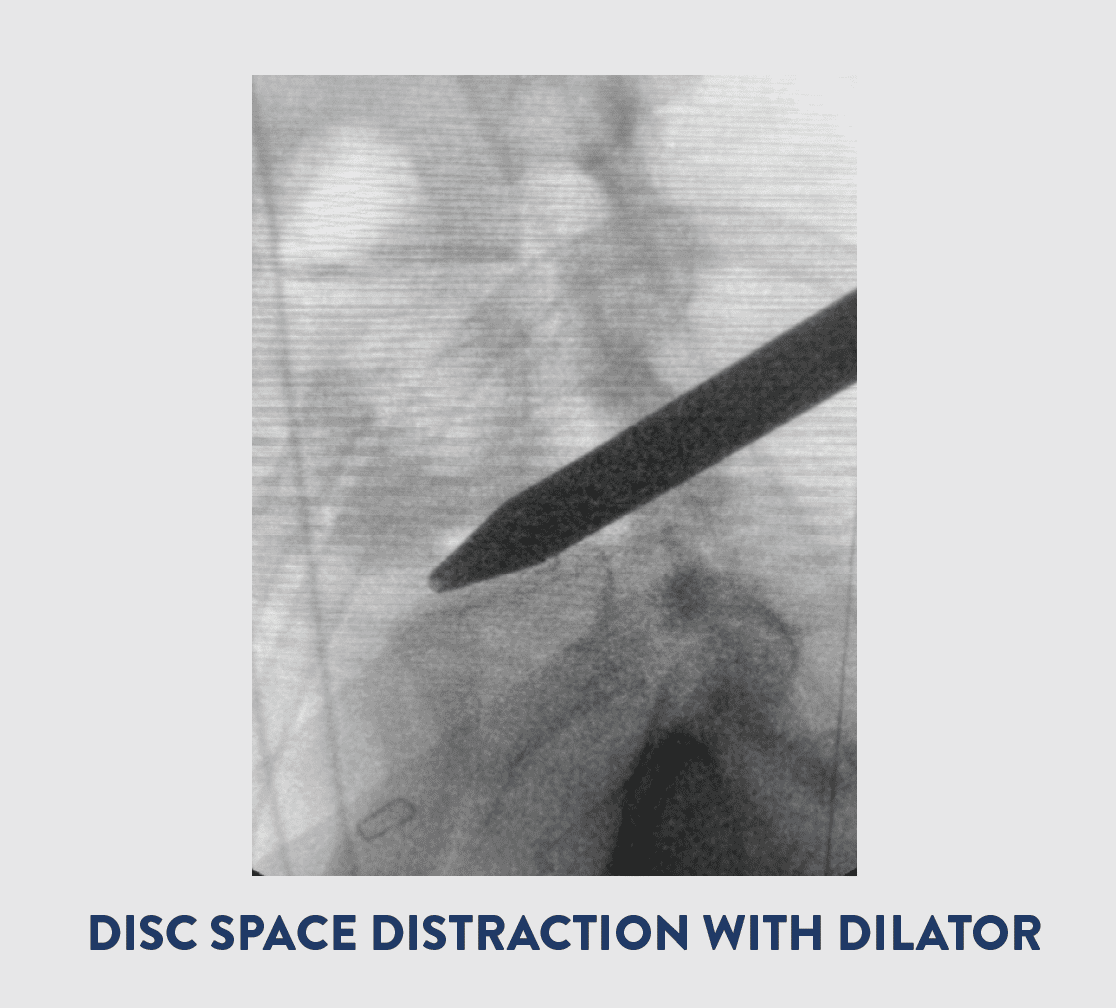
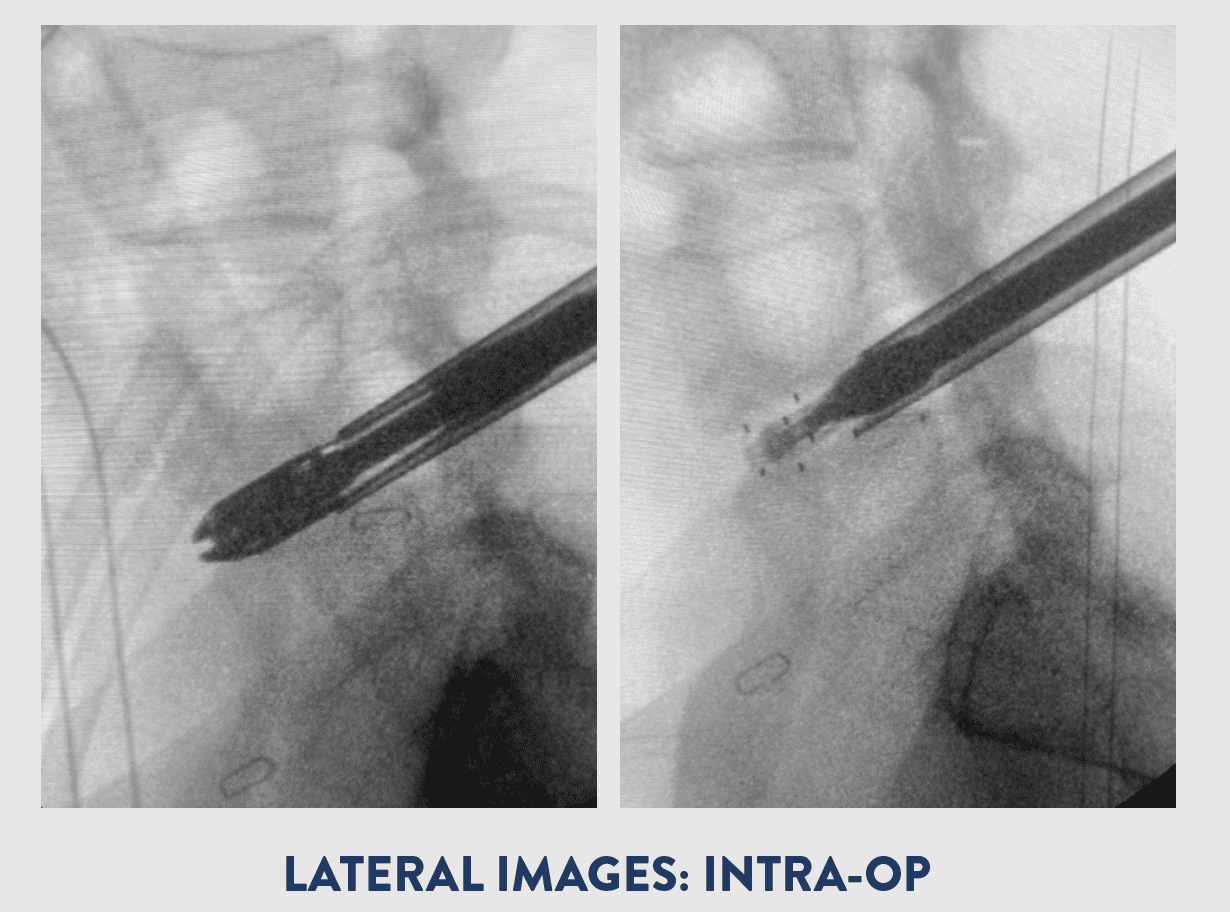
MIS surgery approaches the same problem, but with a different rationale. The goal is to preserve the muscles and tissues through smaller incision and techniques that go through or around the muscles without stripping them off.
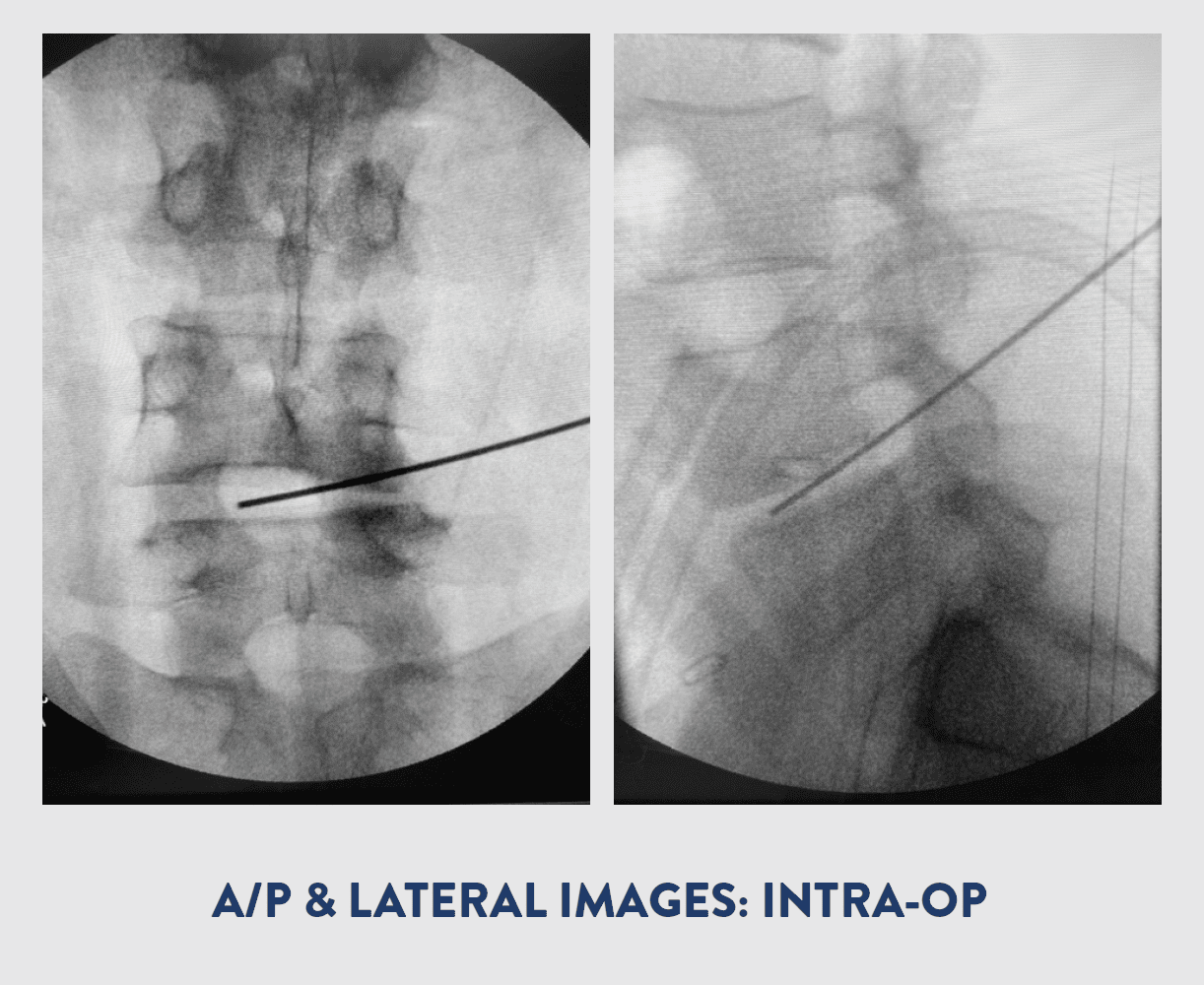
MIS is performed using much smaller incisions than open surgery. Small tube shaped retractors, rather than large muscle dissecting ones, are used to create a narrow opening to accesses the spine. X-ray fluoroscopy and a microscope allow me to visualize the area of interest in the spine.
Very small instruments are used to remove pieces of damaged vertebral bone, cartilage, and/or spinal disc. This type of minimally invasive approach results in less damage to the muscles and soft tissues that surround the spine, which leads to an expedited recovery and less post-operative pain.
What are the benefits of minimally invasive spine surgery?
- Less OR time for procedure
- Faster recovery
- Less bleeding (which means little chance of blood transfusion)
- Smaller incision
- Little or no muscle cutting
- Less risk of infection
- Less pain after surgery
- Decreased reliance on pain medication
- Less rehabilitation is needed
- Patients return to work and activities more quickly
- Less scarring
“MIS surgeries are usually done outpatient which means no hospital stay and getting home that day. This allows me as a spine surgeon to get you back to life much faster!” Dr. Samuel A. Joseph.
Minimally Invasive Surgical Procedures
The following spinal surgeries can be performed using a minimally invasive technique:
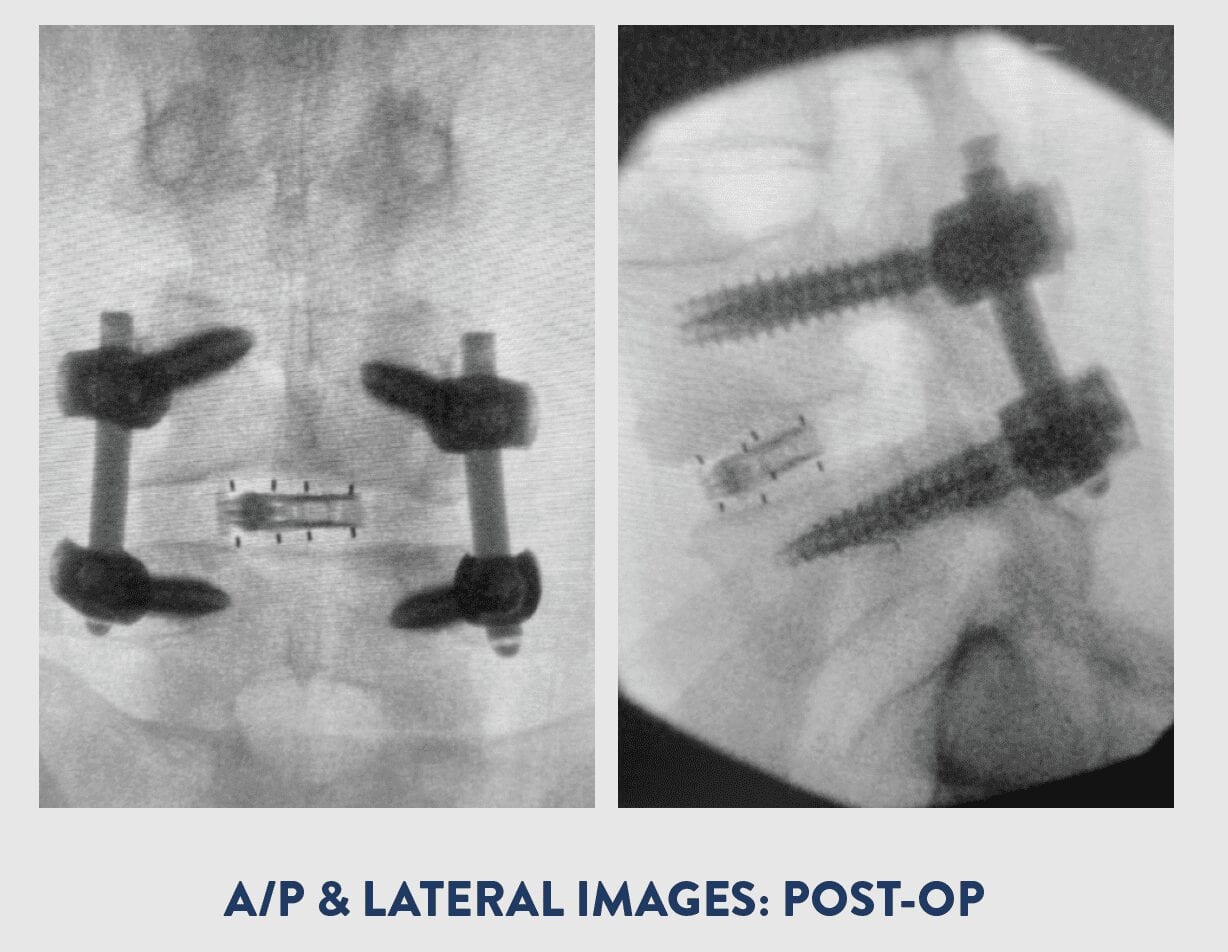
- Spinal Fusion – Spinal fusion is surgery to permanently connect two or more vertebrae in your spine, eliminating motion between them. Spinal fusion involves techniques designed to mimic the normal healing process of broken bones. During spinal fusion, your surgeon places bone or a bonelike material within the space between two spinal vertebrae. Metal plates, screws and rods may be used to hold the vertebrae together, so they can heal into one solid unit.
- Kyphoplasty – Kyphoplasty is a surgical procedure that expands and stabilizes compression fractures of the spine. Kyphoplasty uses a small balloon that gently lifts bone fragments into their correct position. The balloon is inflated to create a space that the surgeon later fills with a special bone cement. The bone cement creates an internal cast that holds the vertebra in place. This extra feature allows kyphoplasty to help restore vertebral height, and thus, help reduce spinal deformity. It also allows a thicker cement to be used which has less risk of leaking out and causing complications.
- Cervical Disc Replacement – Cervical disk replacement surgery involves removing a diseased cervical disk and replacing it with an artificial, man-made device. An artificial disc may be used to replace a disc in either the lumbar spine (lower back) or cervical spine (neck).
- Laminectomy – A laminectomy is a procedure to remove the spinous process and lamina of the affected vertebra. The surgery relieves pressure on the spinal nerve roots by creating more space in the spinal canal. This procedure is primarily performed to relieve symptoms of spinal stenosis.
- Discectomy and Microdiscectomy – Removes either a part of or an entire intervertebral disc to relieve nerve pressure. The difference between the two procedures is that a microdiscectomy is performed using an operating microscope. These procedures are used to remove either ruptured or herniated discs.
- Spinal Cord Stimulation – A pain management technique that involves the surgical implantation of an electrotherapeutic device onto the spinal cord. In the procedure, a device is implanted that introduces low levels of electrical current to the dorsal portion of the spinal cord to block the sensation of pain. Spinal cord stimulators may be a fully implanted system or a system with an external power source.
- Interspinous Spacer Placement – A spacer is an implant that sits between two interspinous processes in the lumbar spine. These spacers are inserted in a minimally invasive procedure. The purpose of interspinous spacers is to increase the space between processes and relieve the symptoms of spinal stenosis
What spinal conditions can be treated with MIS?
- Herniated Disc – A condition in which the annulus fibrosus (outer portion) of the vertebral disc is torn, enabling the nucleus (inner portion) to herniate or extrude through the fibers. The herniated material can compress the nerves around the disc and create pain that can radiate through the back and sometimes down the arms (if the herniation is in the cervical spine) and legs (if the herniation is in the lumbar spine).
- Degenerative Disc Disease (DDD) – A condition in which a damaged spinal disc causes pain. (While everyone has some wear and tear of their spinal discs; not everyone will have pain.) And although it may take decades before you feel pain (if you ever do), the degeneration process can start as early as your 20s.
- Sciatica – Sciatica refers to pain that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. Typically, sciatica affects only one side of your body. Sciatica most commonly occurs when a herniated disk, bone spur on the spine or narrowing of the spine (spinal stenosis) compresses part of the nerve. This causes inflammation, pain and often some numbness in the affected leg.
- Scoliosis, Spinal Deformities – Scoliosis and other types of spinal deformity are characterized by abnormal spinal curves that can vary in size and shape. Normal curvature of spine, called lordosis and kyphosis, naturally occur at different levels or regions of the spinal column. However, scoliosis and/or excessive lordotic or kyphotic curves (eg, hyperkyphosis) are abnormal types of spinal curvatures that can affect balance, flexibility and spinal alignment.
- Spinal Stenosis – A narrowing of the spaces within your spine, which can put pressure on the nerves that travel through the spine. Spinal stenosis occurs most often in the lower back and the neck.
- Vertebral Compression Fracture (VCF) – occur when the bony block or vertebral body in the spine collapses, which can lead to severe pain, deformity and loss of height. These fractures more commonly occur in the thoracic spine (the middle portion of the spine), especially in the lower part.
- Spondylolisthesis – A spinal disorder in which a bone (vertebra) slips forward onto the bone below it.
- Spinal Infections – An infectious disease that affects the vertebral body, the intervertebral disk, or adjacent paraspinal tissue. Spinal infections can develop after a surgical procedure or arise on their own. Infections can affect different parts of your spine—for example, some infections develop in a vertebral body while others may affect an intervertebral disc. Constant back pain without prior injury is a red flag symptom of spinal infection.
- Spinal Tumors – A growth that develops within your spinal canal or within the bones of your spine. A spinal cord tumor, also called an intradural tumor, is a spinal tumor that that begins within the spinal cord or the covering of the spinal cord (dura). A tumor that affects the bones of the spine (vertebrae) is called a vertebral tumor.
Due to the rapid advance in technology new techniques, procedures, equipment and implants are developed to further enhance the treatment of spine disorders and diseases through minimally invasive procedures. However, it is important to note that some severe cases of spinal infections, scoliotic curves, or complex multi-level spinal procedures cannot be treated minimally invasively.
About Dr. Samuel Joseph
Dr. Samuel Joseph is a board certified, fellowship-trained, orthopaedic surgeon who specializes in advanced spine care. He is a leader in new spine medicine techniques and procedures. He is dedicated to pioneering minimally invasive, outpatient spine surgical techniques along with complex scoliosis and revision surgery. Dr. Joseph is among a select group of surgeons to offer cutting edge endoscopic and robotic-assisted surgery for patients to provide the most advanced minimally invasive spine surgery (MIS) available globally. He is also the team spine surgeon for the Tampa Bay Buccaneers.
About Joseph Spine Institute
Joseph Spine Institute is the advanced center for spine, scoliosis and minimally invasive spine surgery. Founded by Dr. Samuel A. Joseph, Jr., a fellowship trained, board-certified orthopedic surgeon. Dr. Joseph has assembled a comprehensive team of highly skilled spine specialists that are devoted to offering the highest level of spine care available today. He has also strategically partnered with some of the most innovative leaders in the spine care industry today in order to bring our patients the latest in technology, products and resources.
From state-of-the-art technology, to alternate therapies and interventional pain management treatments our industry leading spine care practice offers our patients a comprehensive, multidisciplinary approach to diagnosis, treatment and rehabilitation of spinal conditions. Our highly-trained surgeons offer an integrated approach to patients that includes surgical and non-surgical options such as pain management and physical therapy.