Celebrating 5 Years Pioneering Minimally Invasive Spine Procedure
We are celebrating five awe-inspiring years serving spine patients and introducing innovative minimally invasive spine procedures to Tampa Bay.
It is truly a marvel that Joseph Spine Institute has been able to serve countless patients with new minimally invasive spine procedures since our opening in December 2016. We are thankful for all of the invaluable contributions of our staff and the incredible courage and resilience of our spine surgery patients. In honor of them, we are looking back on the past five years, celebrating their accomplishments. Please join us in giving tribute to all the dedicated members of the Joseph Spine Institute.
Opening a practice is often a perilous but worthwhile endeavor. It requires a massive team effort to establish a practice and an even more monumental effort to grow one. With the help of amazing medical professionals, passionate administrators, and devoted team members, Joseph Spine Institute has been able to innovate in incredible ways, serving patients by forging new paths to wellness and health, with new and innovative minimally invasive spine surgery and procedures.
Dr. Joseph and Joseph Spine introduces minimally invasive injection therapy to Tampa Bay
In 2017, Dr. Joseph introduced injection therapy to Tampa Bay, providing a minimally-invasive procedure to help regenerate tissue.
Regenerative Injective Therapy (RIT)is still in 2022 considered a cutting-edge procedure that triggers the body’s natural healing mechanisms, relieving pain and often curing the cause. The emerging field of regenerative medicine features stem-cell-based therapies using autologous platelet-rich plasma/fat/bone marrow which are at the forefront of sports and regenerative medicine worldwide. RIT offers a promising new option for treating those who suffer from chronic back pain.
Regenerative medicine is revolutionizing the treatment of injured tissues as it can completely restore damaged muscles, tendons, and other tissues. Patients may benefit from this groundbreaking, non-surgical, treatment option that relieves pain by naturally promoting long-lasting healing of musculoskeletal conditions.
Dr. Joseph Is Chosen to Serve Tampa Bay Bucs
In 2017, after bringing innovative regenerative spine care to Tampa Bay, Joseph Spine Institute was incredibly humbled to serve our local football team, the Tampa Bay Buccaneers. More than just Super Bowl champions, these athletes are everyday heroes that we are honored to serve.
“I’m excited to be joining the Buccaneer’s medical team, where we focus on providing our athletes the highest level of medical care, utilizing state of the art technology and groundbreaking procedures,
Dr. Samuel Joseph, Tampa Spine Surgeon.
Described as “steadfast and dedicated” for his service to his spine patients, as well as, his humanitarian services to the Make a Wish Foundation, the Butterfly Foundation, and teaching his Minimally Invasive Techniques throughout the world, Dr. Samuel Joseph, of Joseph Spine, has been chosen as the team Spine Surgeon for the Tampa Bay Buccaneers.
Dr. Joseph works with partner Osseus, FDA clears new surgeon inspired device for lumbar fusion
“As a surgeon, it’s very exciting to participate in the device development process and see your ideas brought to life so quickly,” commented Dr. Joseph, founder of Joseph Spine. “Using 3D printing, we were able to go from design to prototype, to finished product much faster than with traditional manufacturing—which means patients get access to more advanced treatments sooner, too.”
Dr. Samuel Joseph. worked alongside medical device firm Osseus Fusion Systems to develop the newly FDA approved 3D printed Aries titanium spinal implants. The approval marks one of the largest FDA clearances for a family of 3D printed spinal devices of that kind.
By partnering with pioneers in the medical industry such as Osseus, Dr. Joseph can offer his expertise as an exceptionally trained spine surgeon to help develop new products and procedures. Combining cutting-edge research with new technology Joseph Spine may offer spine patients new hope for a pain-free life.
Dr. Ron Chatterjee Joins Jospeh Spine Institute
Fellowship-trained, Board Certified Physical Medicine In 2017, we welcomed the talented Dr. Chatterjee to our team. When he joined the practice, he highlighted his unique skill set and perspective. “I look forward to bringing my complimentary skill set to the team”, said Dr. Chatterjee, “My experience in the care of athletes and my expertise in the management of sports-related injuries will contribute to the comprehensive medical treatment the team receives. My goal is to quickly relieve pain and restore function to our athletes.” Dr. Ron Chatterjee, a highly experienced, board-certified physical medicine and rehabilitation physician has been chosen to serve as a team physician for the Tampa Bay Buccaneers for the 2019 season. He joins Dr. Samuel Joseph, founder of Joseph Spine Institute, on the field who is now entering his 3rd season with the Bucs. As a board-certified physician in physical medicine and rehabilitation with a sub-specialty in interventional pain, spine, and sports medicine Dr. Chatterjee brings a unique and multidisciplinary skillset to the team. Chatterjee is highly trained in the treatment and prevention of sports and exercise-related injuries and improving performance.
Dr. Ron Chatterjee
Dr. Chatterjee Team Physician for Tampa Bay Bucs
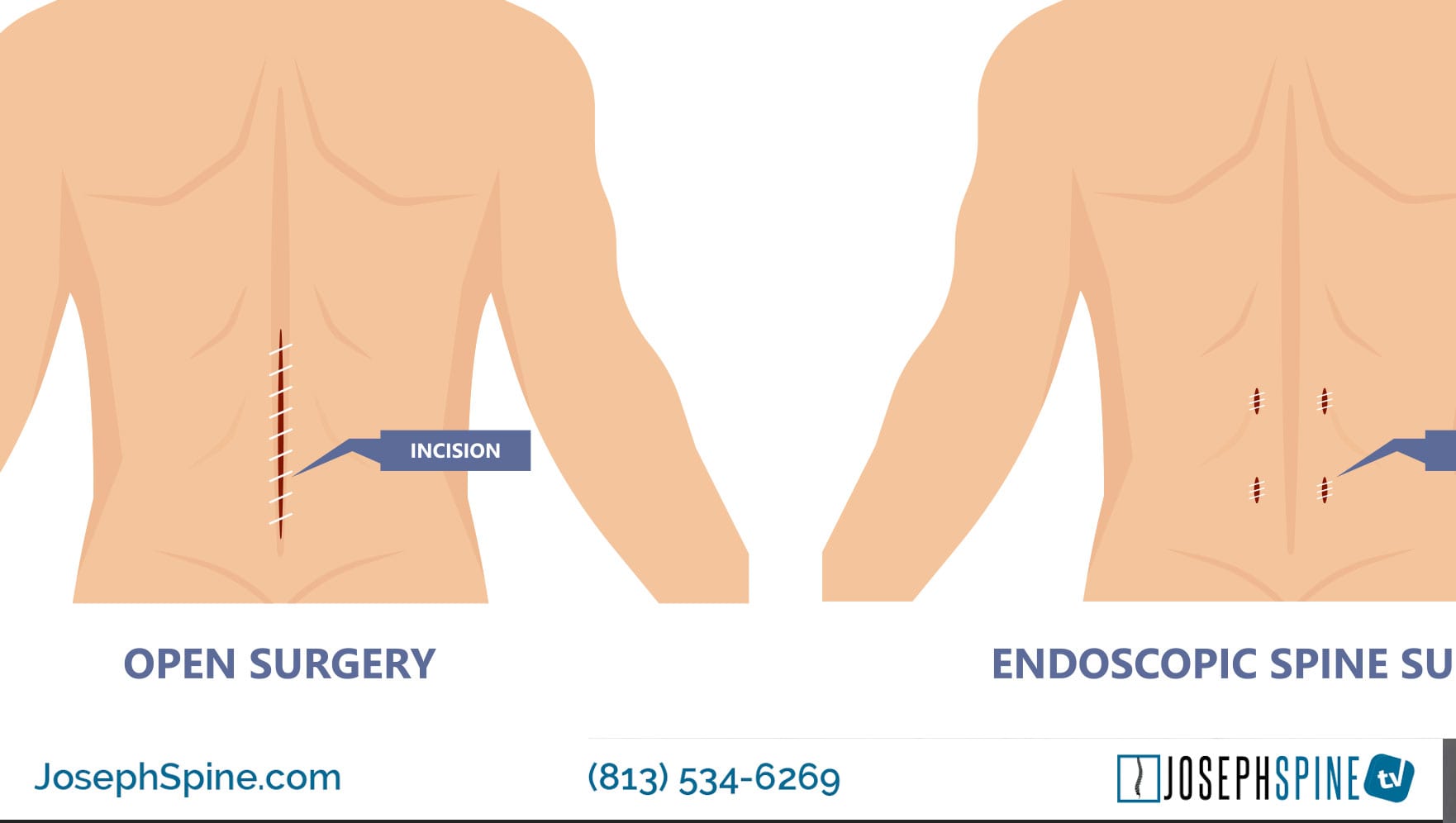
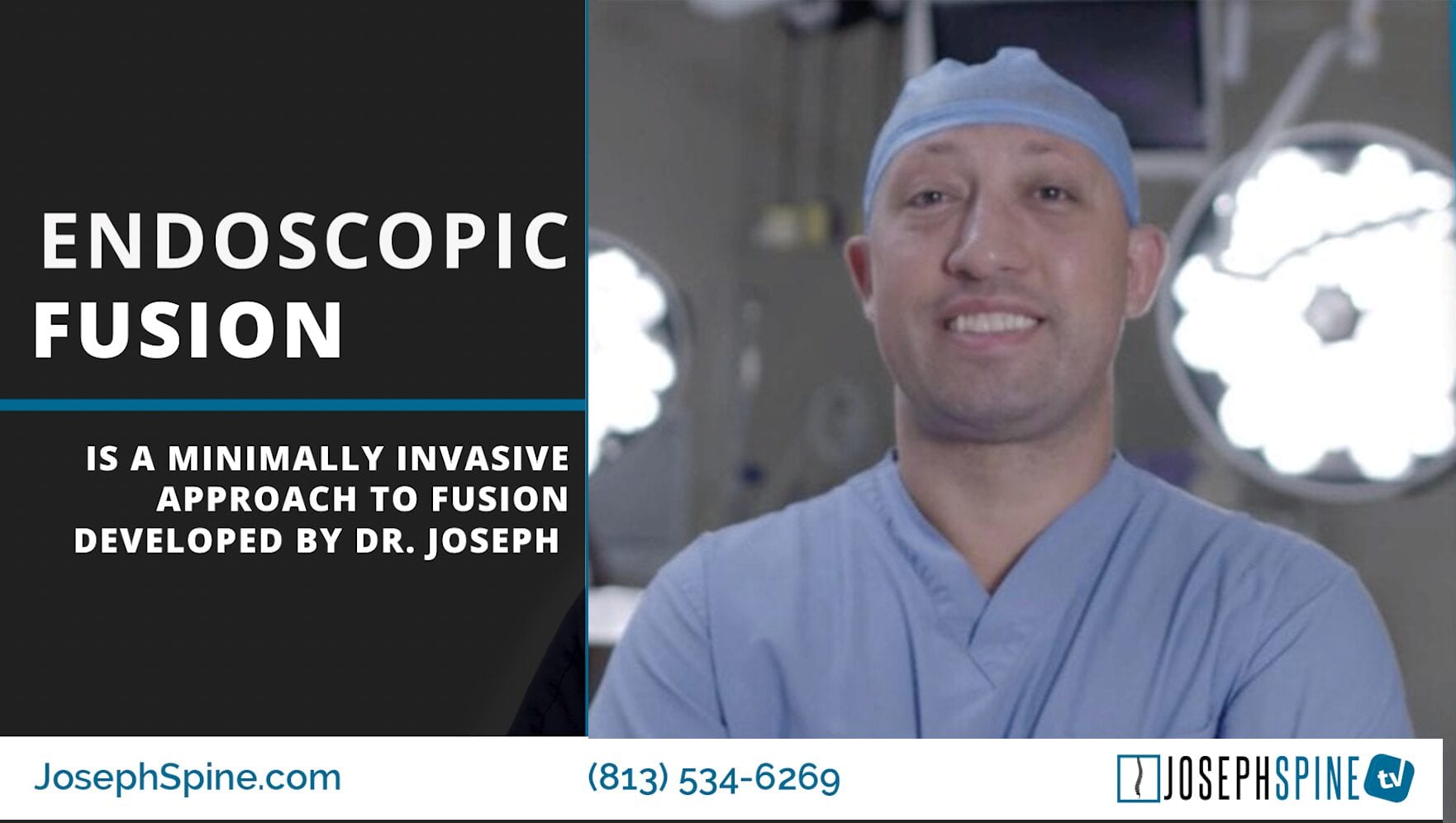
Dr. Joseph Brings a Revolutionary Approach to Minimally Invasive Spine Surgery by Combining Robotic and Endoscopic Technologies
In 2019, our practice brought an innovative new way to approach minimally invasive spine surgery. This revolutionary approach offered new pathways to health, pain-reduction, and recovery for spine surgery patients.
“Together they compliment each other in the perfect package for revolutionizing how spine surgery is done,” Dr. Joseph said. “I am honored to bring this new procedure, combined technology and innovative products to Tampa Bay. At JSI we are dedicated to partnering with the innovators of spine medicine in order to offer our patients the most advanced spine care.”
Partnering with the innovators of cutting edge spine medicine allows JSI to provide our patients with the advantages of next-generation technology that enhances safety and allows for better patient outcomes.
Dr. Joseph Travels to the Dominican Republic to Offer Hope to Patients with Debilitating Spine Conditions
In one of the practices proudest moments, Dr. Joseph helped change a child’s life. Spinal deformities can have a severe impact on everyday life. Debilitating conditions can wreak havoc. That’s why in 2019, Dr. Joseph and a team of talented doctors volunteered their skills to lift people with severe spine conditions out of the debilitating limitations of spinal deformity.
“It felt amazing to have a direct effect on a child’s life and not only improve their appearance but improve their quality of life and life expectancy,” Dr. Joseph told reporters. “Thinking about how many people this child will then affect in their life makes you really take a step back and be humbled by what we as a team are so fortunate and blessed to be able to do.”
In 2019, Dr. Samuel Joseph along with a dedicated team of volunteers traveled to the Dominican Republic over Valentine’s week to save the lives of children and young adults with severe spinal deformities.
The volunteers had a grueling schedule which included 4 to 5 surgeries daily for the week, along with patient screenings and lectures to orthopedic residents.
Joseph Spine Institute Marches for the Make a Wish Foundation
In 2019, our team was driven more than ever to make a real difference in our community.Our entire team walked for the Make-a-Wish Foundation in hopes for a brighter future for those who are suffering.
Walk for Wishes celebrates thousands of wishes that have already been granted while raising funds for future wishes. The event is powered by wish families, volunteers, donors and friends, and participants help to bring the life-changing impact of a wish to children battling life-threatening medical conditions in the Tampa Bay area and surrounding communities in Southern Florida.
In all, everyone came together to raise enough funds to grant 16 heartfelt wishes for kids like 14-year-old Corin who battled leukemia. Her wish was to go on a Mediterranean cruise with her family.
Dr. Thuy Nguyen Joins the Joseph Spine Institute

Dr. Thuy Nguyen
Fellowship-Trained Neurosurgeon
In 2019, we were lucky enough to bring on another talented member to our team, Dr. Thuy Nguyen. Born and raised in the Midwest, Dr. Nguyen graduated from the University of Missouri in Kansas City with two bachelor degrees, one in chemistry and another in psychology.
He went on to obtain his master’s degree in biomedical sciences at the Kansas City University of Medicine and Biosciences where he found a particular interest in anatomy.
Dr. Nguyen would ultimately obtain his osteopathic medical degree from the same university, after which, he completed an internship at the Hillsdale Hospital providing care at a rural and underserved area.
Subsequently, he received his residency training in neurosurgery at Beaumont Health in Detroit; a highly coveted spot as there were only 12 slots in the entire nation for this competitive specialty at the time. He was later named Chief Resident. During his neurosurgery residency,
Dr. Nguyen developed a special interest in the spine and pursued a fellowship in orthopaedic spine surgery at the Oregon Health and Science University (OHSU) where he was immersed in the orthopaedic perspective of spinal surgery and learned from renowned surgeons.
.
Joseph Spine Launches Workers Comp Program
In December of 2019, we still had more work to do. We went to work to make sure our patients could get back to work in a timely fashion. We launched our workers comp program to great success.
Our programs are focused on reducing medical costs and time lost from work, while providing the highest level of care to the patient through our state-of-the-art procedures. We communicate and work closely with employers and case managers to assist patients through the process
Dr. Samuel A Joseph Is Named a Top Doctor in Tampa Magazine
There was no sign of the practice slowing down in 2020. Despite the catastrophic effects of COVID on the globe in 2020, our practice persevered to continue serving our patients in the best way possible.
Dr. Samuel A. Joseph Jr., a leader in minimally invasive spine surgery, and founder of Joseph Spine Institute, was voted by his peers to Tampa Magazines’ 2020 Top Doctors list in the specialty of Orthopedic Spine Surgery for the third straight year in a row.
Dr. Samuel A Joseph Is the First in the Nation to Perform Outpatient PTP (Prone Transpsoas)
2020 was a year that took so many of us aback. We continued to serve our patients and find new ways to forge paths to wellness. In 2021, we took that a step further by doing something no surgeon in the nation had done before.
Dr. Joseph worked in conjunction with other leaders in spine research, development, and technology to bring minimally invasive procedures to complex spine conditions, which in turn results in better faster recovery for patients.
The newly developed procedure performed by Dr. Joseph, PTP (Prone Transpsoas) has many benefits that range from superior surgical efficiency to powerful correction abilities in both the sagittal and coronal planes. PTP allows for the patient to remain in one position for the entire procedure. The prone position creates efficiencies by allowing for a single-position surgery providing simultaneous access to the anterior column and posterior column of the spine.
Dr. Samuel Joseph Brings New Innovative First Awake, Outpatient Spinal Fusion Surgery To Tampa Bay
At Jospeh Spine Institute, we do not merely rest on our laurels. We strive to continually achieve greatness. In 2021, we continued this tradition by bringing another innovative surgery to Tampa Bay.
This new innovative minimally-invasive spine surgery is called an Awake MIS TLIF (transforaminal lumbar Interbody fusion). Dr. Samuel Joseph uses a combination of minimally invasive surgical techniques and advances in anesthetic procedures to offer and bring awake, outpatients spinal surgery to patients in the Tampa Bay Area.
During this procedure the patient is awake, treated with localized pain blocks, avoiding the need for general anesthesia and after-surgery narcotics.
Joseph Spine Institute Welcomes Dr. Anthony Kouri to the Practice
Dr. Anthony Kouri
Fellowship-Trained Orthopedic Surgeon
We experienced even more good fortune in 2021 thanks to our talented team. We were humbled that Dr. Anthony Kouri wished to join our flourishing practice.
“My goal is to always treat each patient’s individual needs and goals. Whether you are a high-performance athlete or simply want to hold your grandchild, I will tailor individualized care to reduce your pain and improve your function so that you may focus on living your life.” – Dr. Anthony Kouri
During his fellowship program Dr. Kouri was exposed to variety of traditional as well as cutting-edge surgical techniques, which trained him for technical proficiency in spinal decompression, spinal instrumentation (both free-hand and using navigation or robotics), and advanced spinal reconstruction techniques (PSO, VCR and multi-level corpectomies). He was also trained in novel techniques such as minimally-invasive spine surgery (MIS TLIF and robotic surgery), lateral access surgery (lateral interbody fusion and ACR) and laminoplasty.
Joseph Spine Institute Celebrates 5 Years of Serving Patients
2022 is full of unknown, but we continue to find new and better ways of serving our patients. We are so thankful to everyone who has contributed to this practice and to all the patients who have courageously sought out treatment. In the next five years, we hope to innovate, empower, and heal more people than ever. Whether it’s through our cutting-edge technology or through our humanitarian efforts, we hope to continue to touch those around us with the power of spine medicine.
About Dr. Samuel A. Joseph, Jr.
Founder, Joseph Spine Institute Dr. Joseph is the founder of Joseph Spine Institute. He is dedicated to pioneering minimally invasive, outpatient surgical procedures. Dr. Joseph is at the forefront of endoscopic spine surgery and a team physician for the Tampa Bay Buccaneers. Dr. Joseph’s practice includes the specialized, conservative, and surgical care of patients. Treatment includes therapeutic injections, disc replacement surgery, minimally invasive techniques, and complex reconstruction of adult and pediatric spinal disorders. Dr. Joseph has used his training and experience to become a leader nationwide on revision surgery for patients who have experienced failed surgery in the past. These patients have traveled to see Dr. Joseph not only from the Tampa Bay area, but from other areas of Florida and across the country as well.
Dr. Samuel Joseph
About Joseph Spine Institute
Joseph Spine Institute (JSI) was founded in 2016 by Dr. Samuel Joseph. He has assembled a comprehensive team of highly skilled spine specialists that are devoted to offering the highest level of spine care available today. He has also strategically partnered with some of the most innovative leaders in the spine care industry today in order to bring our patients the latest in technology, products and resources.
From state-of-the-art technology, to alternate therapies and interventional pain management treatments our industry leading spine care practice offers our patients a comprehensive, multidisciplinary approach to diagnosis, treatment and rehabilitation of spinal conditions. Our highly-trained surgeons offer an integrated approach to patients that includes surgical and non-surgical options such as pain management and physical therapy.