Introducing Joseph Spine Institute’s New Endoscopic Spine Center of Excellence
Innovative Leaders in Minimally Invasive Spine Care: Introducing Joseph Spine Institute’s (JSI) New Endoscopic Spine Center of Excellence
Joseph Spine Institute, a leading provider of comprehensive spine care services, is proud to announce the opening of its new Endoscopic Spine Center. Above all, the center is dedicated to the diagnosis and treatment of spine conditions using minimally invasive endoscopic techniques.
Tampa’s Endoscopic Center of Excellence
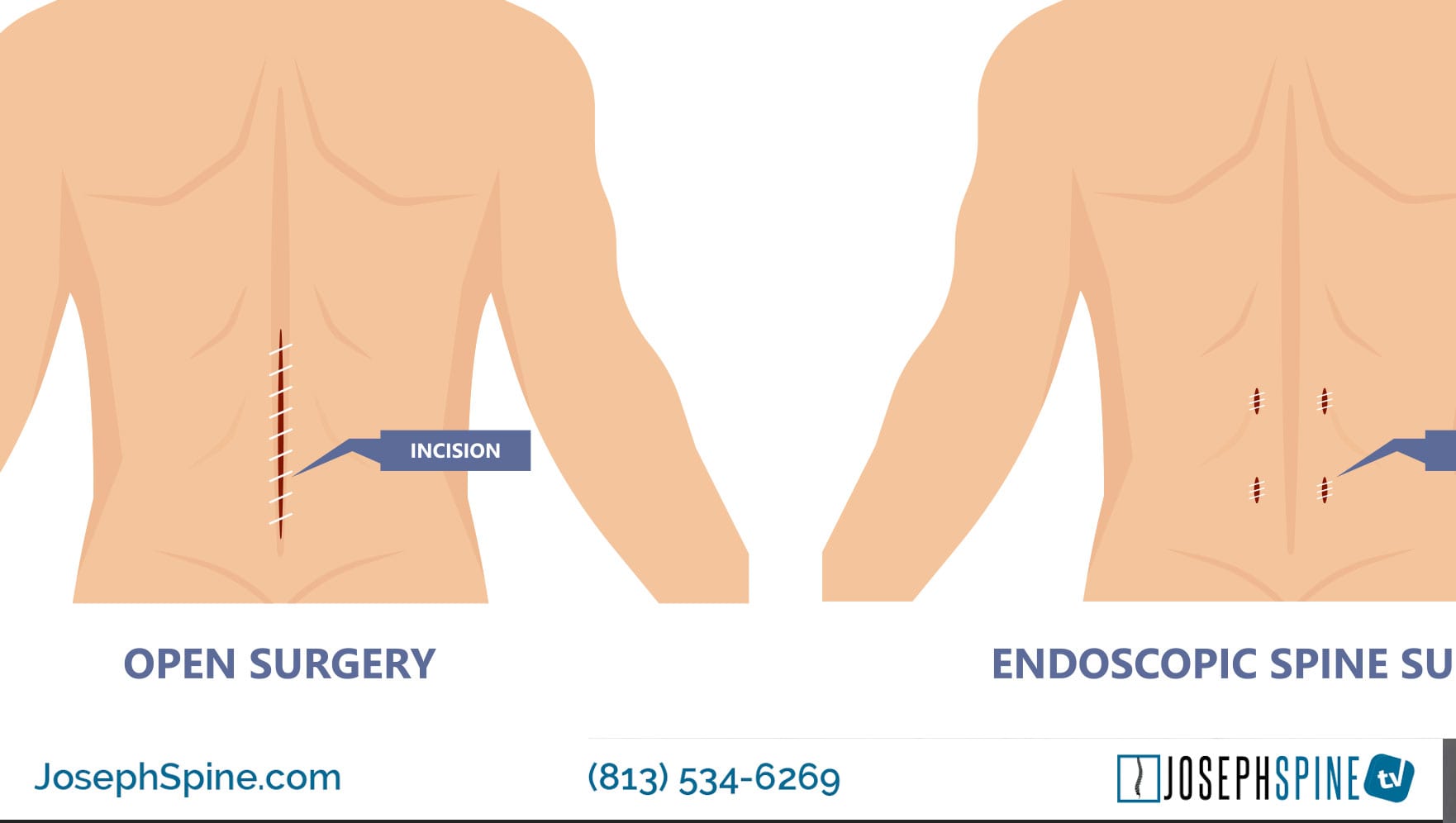
The Endoscopic Spine Center, founded by Dr. Samuel Joseph, is the latest addition to Joseph Spine Institute’s range of services and represents a significant advancement in spine care. With endoscopic spine surgery, patients can benefit from smaller incisions, reduced blood loss, faster recovery times, and less postoperative pain than traditional open spine surgery, as a result patient outcomes and financial expenditure is positively affected. The center isstaffed by the best board-certified spine surgeons who are trained in the latest endoscopic techniques, ensuring that patients receive the highest quality care.
According to Dr. Samuel Joseph, Founder of Joseph Spine Institute, “The opening of our Endoscopic Spine Center represents a significant milestone for our practice. We are proud to be at the forefront of spine care, and we are committed to providing our patients with the most advanced and effective treatments available.”
Key Benefits of Endoscopic Spine Surgery
Key features and benefits of endoscopic spine surgery include:
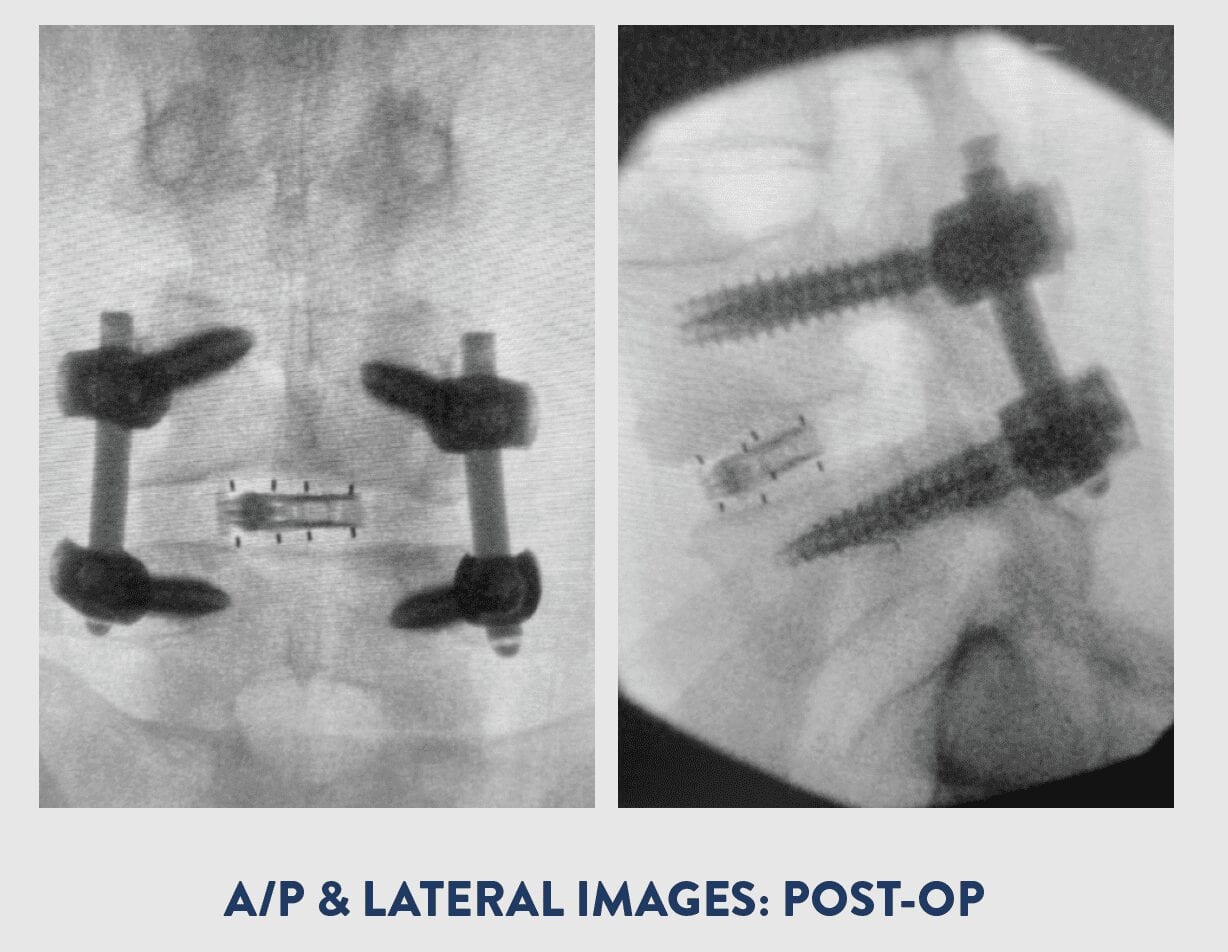
- Minimally Invasive: Endoscopic spine surgery requires smaller incisions compared to traditional open surgeries, resulting in less damage to surrounding muscles and tissues. This often leads to reduced postoperative pain, shorter hospital stays, and quicker recovery times.
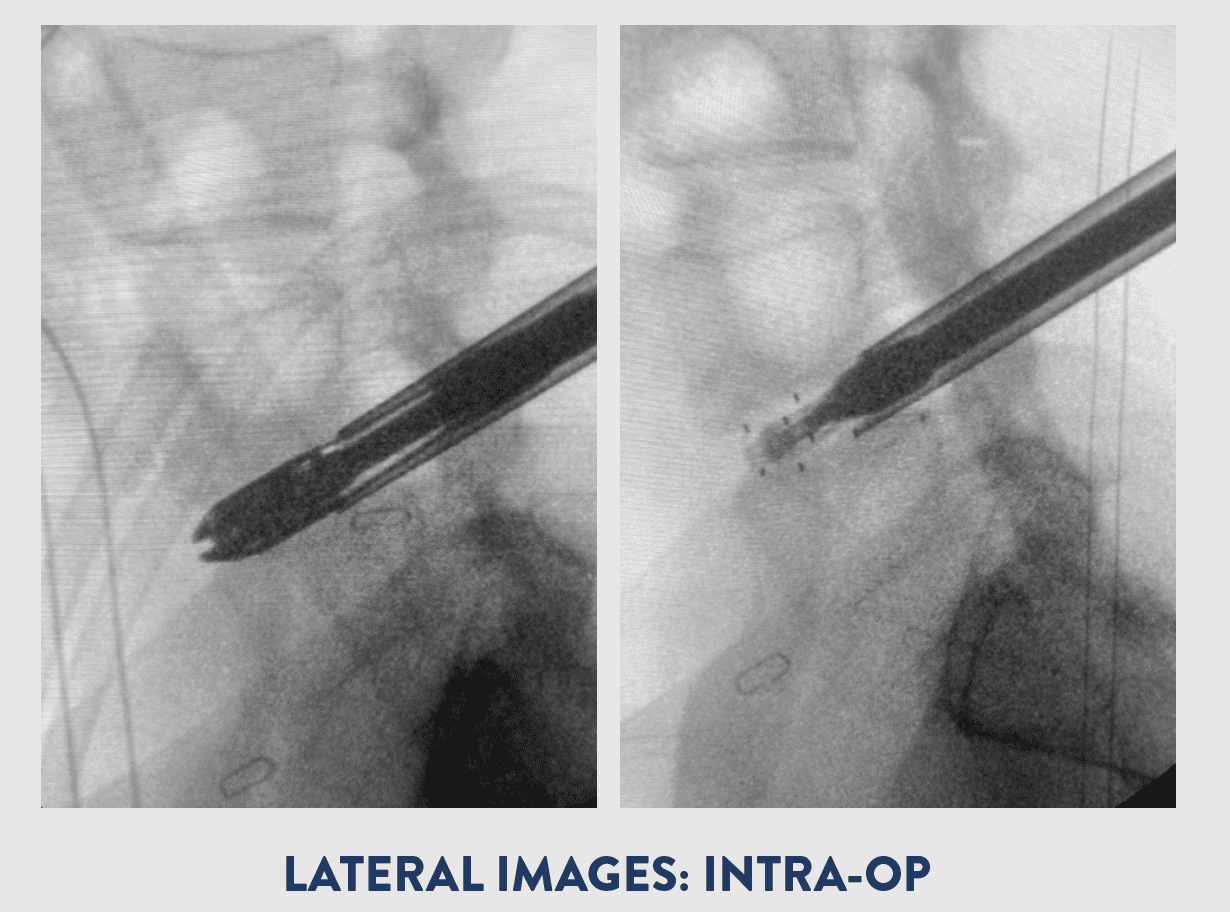
- Precise Visualization: The high-definition camera on the endoscope provides magnified, detailed images of the spine, allowing the surgeon to precisely navigate and perform the necessary procedures with accuracy.
- Targeted Treatment: Endoscopic spine surgery enables surgeons to target specific areas of the spine while sparing healthy tissue, minimizing the risk of complications and maximizing the effectiveness of the treatment.
- Reduced Blood Loss: The minimally invasive nature of endoscopic spine surgery typically results in less blood loss during the procedure, reducing the need for blood transfusions and lowering the risk of complications associated with excessive bleeding.
- Customized Approach: Endoscopic spine surgery can be tailored to meet the individual needs of each patient, with procedures ranging from simple discectomies to more complex spinal fusions, depending on the underlying spinal condition.
- Improved Function: Less healing time. Surgeons often do not have to cut through muscles to complete the procedure, leading to less tissue damage, minimal pain and a quicker recovery.
Offering a Wide Range of Endoscopic Spine Procedures
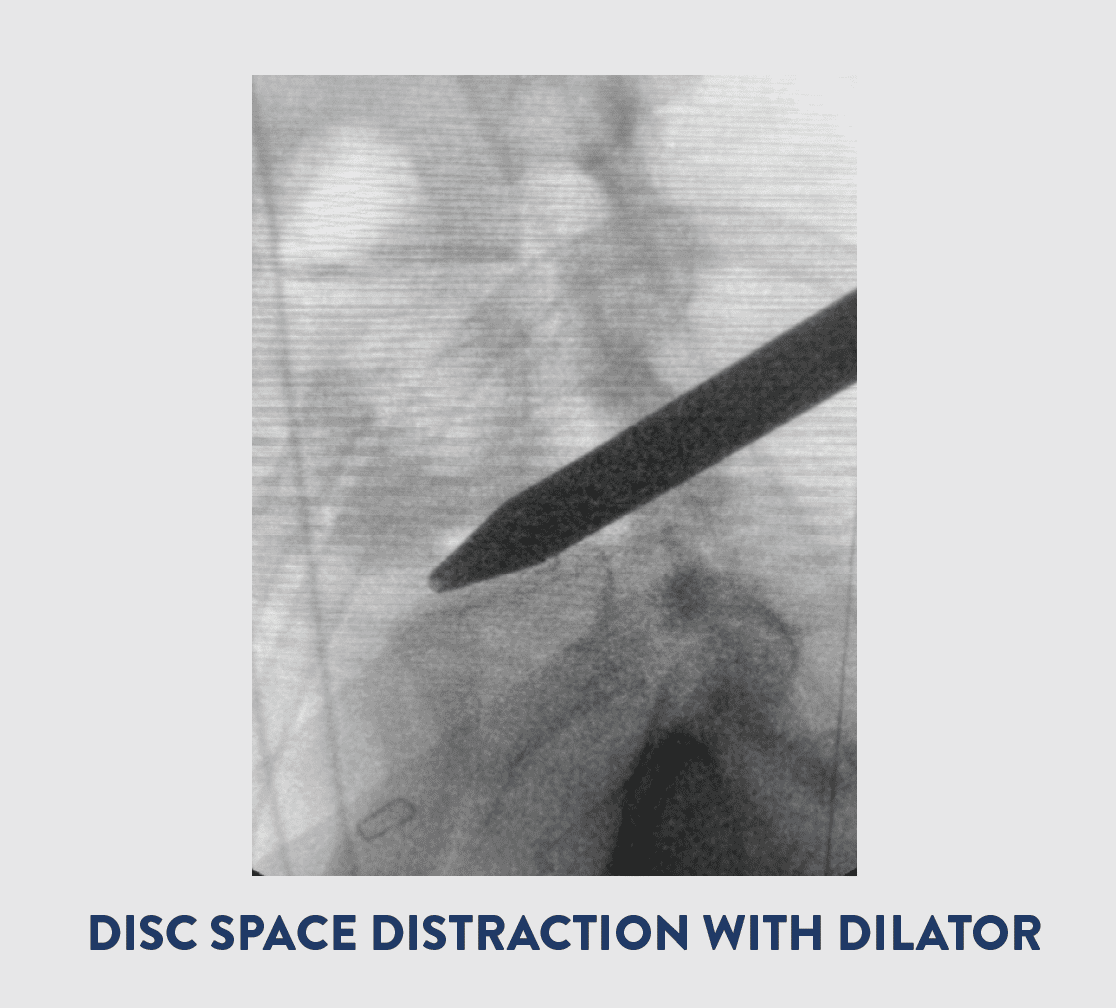
Endoscopic spine surgery, like many minimally invasive spine procedures, is a versatile technique used to treat various spinal disorders and conditions causing back pain or nerve dysfunction.
Determining if you’re a suitable candidate for endoscopic spine surgery depends on factors such as your symptoms, how they affect your daily life, your overall health, and other considerations.
However, due to the benefits of minimally invasive procedures, such as lower blood loss, smaller incisions, and quicker recovery times, endoscopic spine surgery can often be an option for patients who are too ill or frail for traditional open surgery.
For those who are eligible, endoscopic spine surgery can potentially treat conditions including:
- Degenerative Disc Disease: This condition involves the gradual deterioration and stiffening of spinal discs with age, exacerbated by factors like tissue damage, repetitive strain, obesity, improper lifting, sports injuries, and accidents.
- Disc Herniation: Also known as a herniated disc, this occurs when a damaged disc bulges and presses on the spinal cord or nerve roots, causing pain. It can be treated with an endoscopic discectomy, where the protruding portion or the entire disc is removed and possibly replaced with an artificial disc.
- Spinal Stenosis: This condition involves the narrowing of the spinal canal due to bone spurs, which irritate the spinal cord or nerves. Lumbar spinal stenosis affects the lower back, while cervical spinal stenosis affects the neck.
- Spinal Instability: Endoscopic spinal fusion can correct this by using medical hardware to permanently join an unstable vertebra to a stable one.
- Spinal Fractures
- Congenital Spinal Deformities
- Traumatic Injuries: This includes injuries to the vertebrae, soft tissues, or spinal column.
- Spinal Tumors
Endoscopic spine surgery offers a less invasive alternative with numerous benefits for suitable patient
The opening of the Endoscopic Spine Center is a reflection of Joseph Spine Institute’s commitment to innovation and excellence in spine care. The center will provide patients with the most advanced endoscopic techniques, ensuring that they receive the best possible care for their spine conditions.
For more information about the Endoscopic Spine Center or to schedule a consultation, please visit the Joseph Spine Institute website or call (813) 534-6269.
About Dr. Samuel A. Joseph, Jr.
Founder, Joseph Spine Institute Dr. Joseph is the founder of Joseph Spine Institute and the International Spine Foundation. He is dedicated to pioneering minimally invasive, outpatient surgical procedures. Dr. Joseph is at the forefront of endoscopic spine surgery and a team physician for the Tampa Bay Buccaneers. Dr. Joseph’s practice includes the specialized, conservative, and surgical care of patients. Treatment includes therapeutic injections, disc replacement surgery, minimally invasive techniques, and complex reconstruction of adult and pediatric spinal disorders. Dr. Joseph has used his training and experience to become a leader nationwide on revision surgery for patients who have experienced failed surgery in the past. These patients have traveled to see Dr. Joseph not only from the Tampa Bay area, but from other areas of Florida and across the country as well.
Dr. Samuel Joseph
About Joseph Spine Institute
Joseph Spine Institute (JSI) was founded in 2016 by Dr. Samuel Joseph. He has assembled a comprehensive team of highly skilled spine specialists that are devoted to offering the highest level of spine care available today. He has also strategically partnered with some of the most innovative leaders in the spine care industry today in order to bring our patients the latest in technology, products and resources.
From state-of-the-art technology, to alternate therapies and interventional pain management treatments our industry leading spine care practice offers our patients a comprehensive, multidisciplinary approach to diagnosis, treatment and rehabilitation of spinal conditions. Our highly-trained surgeons offer an integrated approach to patients that includes surgical and non-surgical options such as pain management and physical therapy.