Why Scoliosis Awareness Month Matters
Share Your Story for Scoliosis Awareness Month
Why is scoliosis awareness so important? A recent study found that 72% of children and adolescents who wore back braces were able to avoid surgical intervention as opposed to 48% of children who did not wear back braces.
Studies show that early treatment of scoliosis is key
The same study further showed that children who wore back braces for over thirteen hours each day had a success rate over 90%. This provides strong evidence that back braces are an effective non-surgical treatment. However, for back braces to work as a treatment option, the brace must be worn for a significant amount of time. In order for this to be possible, parents have to be educated about the symptoms and screening options available.
Why Scoliosis Awareness Month matters
June is the official month of Scoliosis Awareness. It’s time to speak up about your experiences so we can encourage others to screen for scoliosis. Early detection of abnormal curvature of the spine is key to preventing serious complications. By encouraging others to screen and highlighting educational resources, we can prevent and correct the advancement of scoliosis in our communities.
“National Scoliosis Awareness Month takes place yearly in June with the goal of highlighting the growing need for education, early detection and awareness to the public about scoliosis and its prevalence within the community. The campaign also unites scoliosis patients, families, physicians, clinicians, institutions and related businesses in collaborative partnerships of local activities, events and grassroots networking throughout the month.”
- Scoliosis Research Society
Often, schools offer scoliosis screening. Often, though, these programs do not relay the importance of screening and offer few to no resources that outline how to deal with the news that your child may have scoliosis. Worse still, some school scoliosis screening programs are completely absent.
More people are affected by scoliosis than you might think
Scoliosis affects over 4 percent of the population. While that might not sound like an awfully large number, the rate of degenerative scoliosis, the kind where the spine begins to curve due to age, is present in over half of the senior population. All in all, at least seven million people are affected by scoliosis. It’s one of the most common spine conditions, yet it often goes undiagnosed and untreated.
What causes scoliosis? There are many ways that scoliosis can manifest. It can be congenital, — as in you are born with an abnormal curvature — it can be caused from neuromuscular diseases like cerebral palsy, or it can be caused by spine degeneration or a traumatic injury. There are myriad causes of scoliosis. For this reason, scoliosis is often poorly understood.
What you can do to help
During the month of June, everyone who is or has been affected by scoliosis, from parents of a child with scoliosis to professional spine specialists, speak up about their experiences. By fostering a community and encouraging the sharing of studies, stories, and resources, we can all do our part to minimize the negative effects of scoliosis, not only in our local communities, but all over the globe.
Why we care about Scoliosis Awareness Month
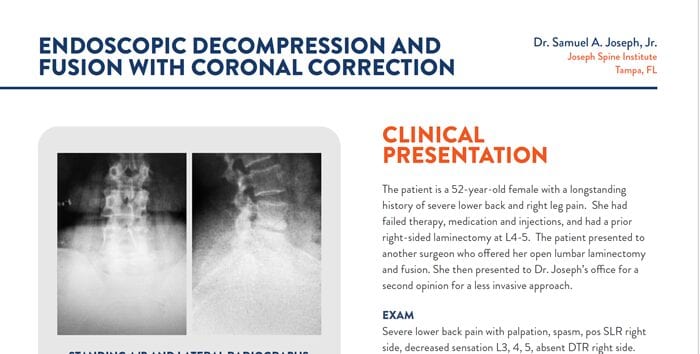
At Joseph Spine, we pride ourselves in our excellent service to patients, providing best-in-class spine surgery and back pain management. We find that preventing the need for surgery is equally important. Eliminating pain and suffering with cutting-edge technology and surgical techniques defines us as a great practice.
Sometimes, cutting-edge technology isn’t necessary, however. Prevention can help your child avoid spine surgery and other invasive producers. Scoliosis, when detected and treated early, can be corrected without surgical intervention. While spinal fusion surgery is certainly an option for those with severe spinal issues resulting from scoliosis, we should all do our part to help reduce the necessity of procedures in cases where early intervention could prevent complications entirely.
Share your story
We encourage you to share your story about scoliosis. As one of the most common spine conditions, we all know someone affected by this condition. We encourage you to share your personal experiences on our social media. Your story is important and will help shape the future of spine health. With your help, we can reduce the pain and suffering associated with scoliosis.